Seminal Analysis (HK$400)
Semen analysis is used to evaluate male fertility a man’s ability to reproduce. This test is also used to assess some genitourinary problems of men as the semen is a combination of secretions from various glands. The test will reveal the healthiness of a man’s genitourinary system.
| Test Item | Test Fee |
| Semen analysis | HK$400元 |
*The fee above does not include doctor’s report explanation. An extra cost of HKD350 will be charged if patients require doctor’s report explanation.
Things you should know for the test
- Collect the semen in a sterile bottle through masturbation. (Collect the bottle in our clinic first). Do not collect it in a condom.
- No ejaculation for 5-7 days before the test. Masturbation to have the specimen in our clinic or at a place where you feel comfortable. Abstinence for too long or too short will affect the quality of semen.
- The sample must be returned to our clinic within 1 hour. Keep the sample close to the body to keep it warm. Do not put it into ice or refrigerator.
The World Health Organization (WHO) has developed the following values for normal semen analysis
| Standard Tests | Normal Values |
| Liquefaction | Within 45 minutes in room temperature |
| Color | Grey-white |
| Volume | 1.5 ml or above |
| pH | 7.0 or above |
| Sperm concentration | 15 x 106 spermatozoa / ml or above |
| Total sperm count | 15 x 106 spermatozoa or above (per ejaculate) |
| Vitality | 58% or above |
| Motility | 40% or above |
| Morphology | 70% or above with normal sperm |
| White blood cells | 0-5/HPF (high power field) |
| Red blood cells | 0-5/HPF (high power field) |
What does the test result mean
Sperm concentration (also called sperm density) is measured in millions of sperm per millilitre of semen. Levels greater than or equal to 20 million per millilitre (and more than 80 million sperm in one ejaculation) are considered normal. The fewer sperm a sample has, the less chance a man has of getting his partner pregnant. A man who has just had a vasectomy would expect no sperm in his sample.
The percentage of moving sperm in a sample is known as its ‘motility’. The more slowly moving or immobile sperm in a sample, the less likely it is that a man could conceive a child with his partner. The progression of the sperm is rated on a basis from zero (no motion) to 3 or higher for sperm that move in a straight line with good speed. If less than half of the sperm are moving, a stain is used to identify the percentage of dead sperm. This is called a ‘sperm viability test’.
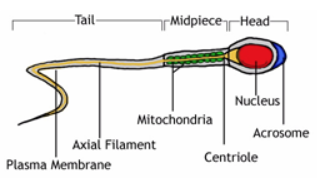
Morphology analysis is the study of the size, shape, and appearance of the sperm cells. The analysis evaluates the structure of 200 sperms, and any defects are noted. The more abnormal sperms that are present, the more the likelihood of infertility.
Several factors can affect the sperm count and other semen analysis values. A man may have a lower sperm count if he has physical damage to the testicles, has gone through radiation treatment of his testicles, or has had exposure to certain drugs (such as azathioprine). A man with a higher level of oestrogens may have a lower sperm count.
Some of the common causes of male infertility are extremely high fever, testicular failure (failure of the testicles to produce sperm), obstruction of the tubes that carry semen to the penis, and a less than normal amount of sperm in the sample (oligospermia).
Normal Structure of a Sperm
Sperm under Microscope